You find A Remedy Transitions Into The Killer
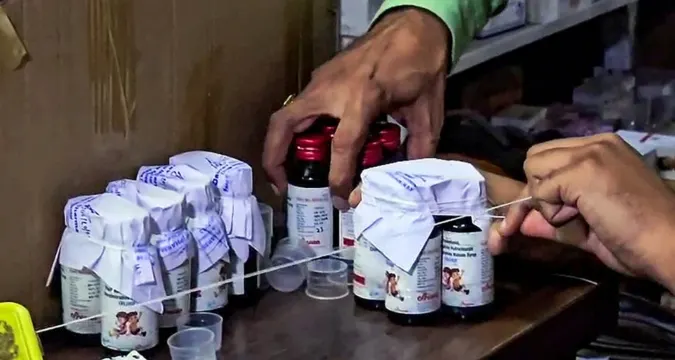
The loss of life associated with a toxic cough syrup has already reached 17 children in the regions of central India in one of the most shocking health tragedies in recent history. At higher levels many times higher than the acceptable level, a syrup, Coldrif, is suspected to include diethylene glycol (DEG), a chemical commonly employed in industrial antifreeze. Physicians report that the drug has permanently impaired brains and kidneys of some of the victims.
Once the nation saddens down, another troubling reality is revealed by the tragedy: the system of pharmaceutical regulation in India is not working where it is most needed by the nation, the safety of Indian children.
The Tragic Timeline: The Way The Deaths Lost Gravity.
The initial toddlers with the onset of unidentified spontaneous kidney failure in Chhindwara district, Madhya Pradesh, left the doctors perplexed first. The symptoms started with fever, vomiting, fatigue, though soon started to intensify into seizures, respiratory distress, loss of consciousness.
During the six weeks, 17 kids ranging in age between one and four years lost their lives in Chhindwara and Nagpur hospitals. Local health departments confirmed that they had all been given the same make of cough syrup, Coldrif.

Analysis of the specimen in a lab, later, displayed the nightmare statistics: the diethylene glycol in the syrup was 48.6%, which is approximately 500 times that of the safe limit. By October 2025, at least 11 other children are in a critical condition with similar symptoms.
The Chemical Offender: The Diethylene glycol (DEG)
What Is Diethylene Glycol?
Diethylene glycol is a tasteless, solid liquid that is used as a solvent in brain fluids, paints, and antifreeze. As a pharmaceutical ingredient, sometimes it contaminates or can be fraudulently replaced by propylene glycol, a safe solvent employed in syrups and elixirs.
Minimal amounts of DEG are fatal, particularly in infants and young children. After absorption, it is metabolized into di-glycolic acid that leads to acute kidney and brain injury.
The Effect of DEG on the human body
Renal damage – DEG mainly assaults renal tubular cells, inducing acute renal failure and total closure of urine production in just a few days.
Brain Injury – The chemical bypasses the blood-brain barrier resulting in encephalopathy, seizures, and permanent neuronal damage.
No Antidote – Medical specialists underline that there exists no single antidote; even dialysis or intensive care is not much successful when brain damage is already received.
According to the doctors of Nagpur Government Medical College, the situation was very simple, when it comes to prognosis of DEG: once it has made it to the brain it is all about giving the patient some comfort care, however it is not reversible.
Field Site: Chhindwara District of Madhya Pradesh
The Chhindwara district has turned into the ground zero in this emerging health crisis. Early probings showed that stocking of Coldrif bottles occurred in local pharmacies and unregistered medical shops along tribal and rural belts.
Unconscious of the actual threat, parents administered the syrup to their children as a normal home remedy to curing the common cold and cough in their toddlers, one of the household rituals in rural India.
Local hospitals were overrun as children started collapsing 48 hours after administration. Although emergency personnel needed to transfer those to Nagpur and Bhopal, many of them could not be saved.
Since then, the state government prohibited the sale of all Coldrif batches and gave an immediate recall of the product.
The Regulatory Failure: Oversight in the Blind
Weak Pharmaceutical Audits
The Indian pharmaceutical industry has a world wide reputation in terms of generics; however, regulation hastens out to pace faster growth. Quality audits are often evaded in small-scale manufacturers under systems of loan licenses.
Professionals indicate that state drug controllers do not have the manpower nor modern laboratories to test product composition routinely, which creates loopholes in testing that pose danger.
Defective Raw Material and Light-minded Procurement.
The preliminary investigations raise the possibility that the contamination source is a bad supplier of solvents who might have been replacing DEG with propylene glycol, because of the price divergence. This is due to delays in batch-level validation which allowed the filtering toxin to go down the production line.
This breakdown is a symptom of a long line of laxity – the chemical producer/supplier, the chemical producer distributor and retailer.
Divisional Control and Delayed Recollection
The dual-layered regulatory infrastructure in India; central (CDSCO) and state-level drug control has been seen to face coordination issues in the past. When recall orders have been issued, the thousands eaten bottles or sold off-the-grid in the informal markets are already consumed.
The Human Toll: Grief, Guilt, Angry, Public.
Stories From The Families
Meera Yaduvanshi, who had a two-year-old son Jayashu among two offspring, tells her nightmare in Chhindwara Parasia block:
“He had just a little cough. Syrup, two spoons of syrup, Doctor. He began not to pass urine the following morning. Within two days, he was gone.”
One of the others, Ramesh Pawar, claims to have stood on top of his son, Vedansh, and endured the terrible scenes of watching him forcefully convulsing and then going into a coma.
To such families, mourning has become rage. They want more than justice, they want structural change – Meera says, as she holds on to both her children, medical report in her hands, No one else can be as we have been.
Doctors Under Pressure
Physicians who treat the victims say it puts a massive emotional and ethical pressure. One elderly doctor of Nagpur GMC stated, we had been treating unknown poisoning initially. It wasn’t until later that we discovered that the same cough syrup was universal with all the cases.
The discovery caused a great frenzy among health care professionals with most of them halting their prescription of local syrups at once until they got a better understanding.
The Long War on Drug Contamination in India
This is not a one off occurrence. The decades of pharmaceutical catastrophes in India have had several instances of medicine contamination:
- 1998, Gurgaon: 33 kids killed in ingesting DEG-laced cough syrup.
- Jammu, 2019: 12 dead children were a result of poisoned Coldbest syrup.
- Gambia, 2022: 66 child deaths were associated with Indian-made cough syrups used in countries worldwide.
- 2023, Uzbekistan: 18 children were poisoned with imported Indian syrups used by DEG.
Every event elicited a spurt of disillusionment that did not produce any significant policy change. Domestic vigilance is weak in spite of global caution.
The Science Of Preventability: How Quality Testing Could Have Saved Lives
Drug analysts maintain that it would have been with very simple routine gas chromatography (GC) testing that DEG contamination would have been easily observed. This technology is available in the majority of government laboratories, but the issue is that most people have inconsistent testing and short cuts in their procedures.

Had each batch of syrup been tested prior to being released, and not only the initial one, the contamination may have been detected in the early stages. Moreover, by using automated barcoding systems that trace data of batch-to-retail distribution, immediate recalls would be possible.
Nevertheless, several smaller companies still go to work under self-certification with minimal government cross-checking – a structural vulnerability that exposes the population.
Investigations and Accountability Fallout of the Law
This has prompted a countrywide investigation by the Drug Controller General of India (DCGI). Section 274 and 304A of Indian Penal Code against causing death by negligence may be heaped upon the manufacturing company, the name of which is, as yet, official and is being investigated.
Authorities in the Central Drugs Standard Control Organization have placed the production department under a seal, and analysis is being re-done in three other laboratories.
According to legal experts, although arrest can be done, international law has no specially prepared pharmaceutical homicide law; this means that criminal charges can be brought directly against criminals in India. This legal loophole has continued to allow careless manufacturers get away with fines or suspended licenses.
The choke point of both Cheap Drugs and the Thousand and One Nights presented at full length Dilemmas.
The pharma paradox in India is basically dominated by one hard question, which is how to make both cheap and safe at the same time. The low cost drug ecosystem in India is a blessing to millions of people, yet as competition on price slashes battalions, quality benchmarks were compromised.
It is the fear of analysts in public health that until India develops a culture of ethical compliance, and not only reactive implementation, these kinds of tragedies can be repeated still.
A high level WHO consultant refers to India as the pharmacy of the world and our home regulatory culture has to govern that international accountability.
What Has to Be Done: A Plan of Reform
- Enhance Surveillance Regulation.
- Implement mandatory third party audibility of all pediatric and OTC formulations.
- All test reports go through a central portal that goes public.
- Do not impose at all temporary suspension of repeat violators, but lifetime bans.
- Increase Supply Chain Transparency.
- Introduce QR traceability indications on each bottle.
- Require tamper-proof seals and verification of retailers prior to sale.
- Use SMS and regional radio to publish public alerts in the event of a recall.
- The reforming of legal accountability.
- Develop a Pharmaceutical Manslaughter Act that makes wrongful drug-related deaths a criminal offense.
- Establish a fast-tracking consumer court to deal with a medical negligence-related issue.
- Usurer victim compensation welfare through industry pools.
- Train The Society and the health care workers.
- Training of rural doctors to detect symptoms of chemical poisoning at the earlier stages.
- Organize community sensitization on counterfeit and substandard medicines.
- Introduce nursing and medical training on drug safety.
- Invest In Infrastructure Testing.
- Have at least one specialized testing laboratory in each district.
- Encourage open interactions between the government and industries to encourage quality control in analytical control.
- Implement AI-based detections in case of anomalies with chemical compositions.
The Road Ahead: Reform, Accountability and Reconstruction
India is at a turning point. The Coldrif tragedy should be a wake-up call at the national level, a striking opportunity to reform old systems and to punish irresponsible parties and reconstruct the public distrust towards the sphere of medicine.

Justice can be delayed in the eyes of the parents of 17 dead children. Yet when their outrage brings reform there is nothing to lose in the losing.
According to one of the pediatricians of Nagpur:
“These children paid the price for the system’s neglect. The least we can do is ensure no other parent has to bury a child because of a cough syrup.”
Since Grief To Reform: A Nation Of Reckoning
This is not just the story of tainted pharmaceuticals, but a tale of general indifference, moral dissipation, and shaky confidences. The healthcare ecosystem set up in India, which is globally admired in its extent, will have to look deeply in.
In their call to regulators, policymakers, and leaders in the industry, The Vue Times urges them to find a common purpose of one goal: Never Again.
As long as accountability is not as natural as affordability is, the dream of having safe medicine to all will be incomprehensibly disappointing.








